What is cervical cancer?
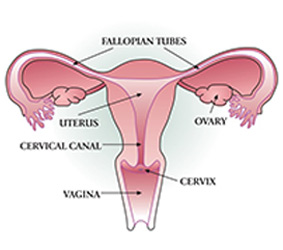 Cervical cancer is cancer of the cervix. Only people who have a cervix* (a body part that connects the uterus, or womb, to the vagina, or genital opening) can get cervical cancer. Cervical cancer is almost always caused by human papillomavirus (HPV). HPV is a virus that is most often passed from one person to another through sexual contact. Sexual contact includes any time another person has contact with your genitals (private parts). This contact can be with the hands, mouth or genitals.
Cervical cancer is cancer of the cervix. Only people who have a cervix* (a body part that connects the uterus, or womb, to the vagina, or genital opening) can get cervical cancer. Cervical cancer is almost always caused by human papillomavirus (HPV). HPV is a virus that is most often passed from one person to another through sexual contact. Sexual contact includes any time another person has contact with your genitals (private parts). This contact can be with the hands, mouth or genitals.
HPV is common and 8 out of 10 people will get HPV at least once in their lifetime. There are more than 100 types of HPV, which can cause changes to the cells of the cervix. HPV will often go away on its own without doing any harm, but the cell changes from some types of HPV can turn into cervical cancer over time if they are not treated. Regular cervical screening can find types of HPV that can sometimes cause cervical cancer. Cervical screening also checks for cell changes in the cervix caused by these types of HPV before there are any symptoms. These cell changes can be treated before they can cause cervical cancer.
Cervical cancer is almost always preventable with regular screening, more testing after abnormal results (if needed) and HPV vaccination.
*The source of data used in the My CancerIQ Cervical Cancer Risk Assessment is based on people who were assigned female at birth. Because of this, gender binary language (male, female, man, woman) may sometimes be used. If your gender is different from your sex assigned at birth, My CancerIQ may not assess your risk accurately. Talk to your doctor or nurse practitioner about your personal risk of developing cervical cancer.
Risk factors that increase the risk of getting cervical cancer
Cervical cancer risk factors are things that can affect the risk of developing cervical cancer. Some of these risk factors can be changed, but some cannot.
Being exposed to human papillomavirus (HPV) is the biggest risk factor for cervical cancer because it is almost always caused by HPV. HPV is a virus that is most often passed from one person to another through sexual contact. Sexual contact includes any time another person has contact with your genitals (private parts). This contact can be with the hands, mouth or genitals.
Keep reading below for more information on how to lower your risk of getting cervical cancer by changing certain risk factors.
Sexual activity
Some studies suggest that people who had sexual contact for the first time at a younger age or who have had many sexual partners over the course of their lifetime may have a higher risk of getting an HPV infection. The exact reasons for this finding are not clear. It may be that these people have a higher chance of having a sexual partner with HPV. But no matter when someone starts having sexual contact, it is recommended that they start cervical screening no earlier than age 25.
Use of condoms
Some research shows that using condoms regularly may help lower the risk of developing cervical cancer by lowering exposure to HPV. But condoms do not completely protect against HPV or fully prevent cervical cancer.

Smoking
People who smoke cigarettes and become infected with a type of HPV that can sometimes cause cervical cancer have an up to 80% higher risk of developing cervical cancer compared to people who do not smoke cigarettes. Smoking weakens the immune system, making it harder for the body to get rid of infections. Cigarette smoke also has over 70 carcinogens (chemicals that can cause cancer) that increase the risk of developing many forms of cancer by damaging the DNA in cells, preventing the body from getting rid of damaged cells or affecting normal cell growth.
Giving birth
Some studies suggest that people who have given birth may have a higher risk of developing cervical cancer, which may be due to a higher exposure to HPV with sexual activity, possible damage to the cervix during childbirth, hormonal changes during pregnancy or more cervical screening with pregnancy. It is also harder to diagnose cervical cancer and for the body to get rid of an HPV infection during pregnancy. Cervical screening is safe in pregnancy and pregnant people should be screened if they are due for a test.
Sexually transmitted infections (STI)
Some studies suggest that having an HPV infection at the same time as STIs, such as genital herpes and chlamydia, may increase the risk of having an HPV infection that does not go away. Having some STIs, such as the human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), may also affect the immune system and make it harder for the body to get rid of an HPV infection. HPV infections will usually go away on their own, but if they do not, they can cause changes in the cells of the cervix that can turn into cancer if not treated.
Being immunocompromised
Immunocompromised people have a weakened immune system. These people include anyone who is living with HIV/AIDS, takes medicine that makes the immune system weaker or needs dialysis. Someone is also considered immunocompromised if they have organ or stem cell transplants, lupus or congenital immunodeficiency (born with an immune system defect). These conditions, diseases or medicines that make the immune system weaker can make it hard for the body to get rid of an HPV infection.
If you are immunocompromised, talk with your doctor or nurse practitioner about cervical screening. You may need to get cervical screening every 3 years if you have a weakened immune system.
What you can do to protect yourself

Screening:
The Ontario Cervical Screening Program
The Ontario Cervical Screening Program is a province-wide screening program that recommends that anyone with a cervix (women, Two-Spirit people, transmasculine people and nonbinary people) who has ever had sexual contact and does not have any possible cervical cancer symptoms should get cervical screening every 5 years starting at age 25. Some people may need cervical screening every 3 years if they have a weakened immune system, such as people living with human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) or who have had an organ transplant.
You should still get screened if you:
- Have had the human papillomavirus (HPV) vaccine.
- Feel healthy.
- Have been through menopause.
- Have not had any family members with cervical cancer.
- Have had sexual contact with only 1 person.
- Have had the same sexual partner for a long time.
- Have not had sexual contact in a long time.
- Are in a same-sex relationship.
Most people can stop cervical screening if they have had 1 normal HPV test result anytime from age 65 to 69. But some people need to be screened until age 74, including people who:
- Were not screened from age 65 to 69.
- Are immunocompromised.
- Were told by age 69 that they can stop colposcopy, but need to be screened more often.
If you have had a hysterectomy you should talk to your doctor or nurse practitioner to see if you need to keep getting cervical screening.
If you have not been screened for more than 5 years, talk to your doctor or nurse practitioner.
How to make an appointment for your cervical screening test:
- Call your doctor or nurse practitioner to ask them to do your test.
- To find Indigenous primary health care organizations, visit Indigenous Primary Health Care Council and Association of Family Health Teams of Ontario.
- Use Health811 any time to find a clinic that does cervical screening tests:
- Call 811 (TTY: 1-866-797-0007).
- Use the live chat at ontario.ca/health811.
- Search for “cervical screening test” on the “Find a service” page of ontario.ca/health811.
To find out more about the Ontario Cervical Screening Program and cervical screening:
- Visit ontariohealth.ca/cervical-test for more information about cervical screening.
- Visit Ontario Cervical Screening Program or call 1-866-662-9233.
- Find information for First Nations, Inuit and Métis people on cancer and cervical cancer screening:
- Cancer 101 Toolkit – use it to learn, or help others learn about the basics of cancer, how to prevent it and treatment.
- Cervical Screening Fact Sheets – for First Nations, Inuit and Métis.
Vaccination
In Ontario, a provincial immunization program for the HPV vaccine is delivered through schools to all Grade 7 students for free. This program is designed to prevent certain cancers, including cervical cancer, by vaccinating people before they have their first sexual contact and are potentially exposed to HPV.
Learn more:
- Visit the Ministry of Health’s website to find out more about Ontario’s HPV Vaccination Program.
- Call Health811 at 811, TTY 1-866-797-0007.
Although the HPV vaccine is very good at protecting against some types of HPV that can sometimes cause cancer, it does not replace cervical screening. The HPV vaccine does not protect against all cancer-causing types of HPV and does not protect against HPV infections people may already have before getting vaccinated. Therefore, people age 25 and older with a cervix who have ever had sexual contact with another person should get regular cervical screening to prevent cervical cancer, even if they got the HPV vaccine.
Safer sexual contact
HPV is a virus that is most often passed from one person to another through sexual contact. Sexual contact includes any time another person has contact with your genitals (private parts). This contact can be with the hands, mouth or genitals. If you feel uncomfortable talking about sexual health with your intimate partner or partners, you are not alone. Many Ontarians are reluctant to ask partners to use condoms or talk about their sexual history. But such conversations are important for your health: having unprotected sex, especially with multiple sexual partners, may increase your risk of HPV infection and other sexually transmitted infections. Sexual health clinics have objective, confidential and compassionate professionals who will listen to you and help you. You can also talk to your doctor or nurse practitioner for more information. It is important to know that condoms do not completely protect against HPV or fully prevent cervical cancer, so you should still get screened if you are due for a cervical screening test.
Learn more:
- To find a sexual health clinic at your nearest public health unit or community health centre, visit the Ministry of Health website or contact Health811 at 811, TTY 1-866-797-0007.
- Visit SexandU.ca.

Become smoke-free
Cigarette smoke – whether it is your own or someone else’s second-hand smoke – can affect your immune system, damage DNA and increase the risk of developing cancer. Even if you see yourself as a person who smokes, you can change that. Over half of people in Ontario who have ever smoked have been able to quit. Of the people who still smoke, nearly half try to quit each year. Sometimes, people need to try quitting several times before they become permanently smoke-free. Each time you try to quit smoking, you move closer to your goal of being smoke-free.
Tips if you are thinking about quitting now or soon
- There is no one “right” way to quit. Different people may use different approaches, so it is good to learn about all of your options. For example, nearly 6 out of 10 people who try to quit smoking use something to help them, such as nicotine replacement therapy, prescription medications, calling telephone quit lines or taking a smoking cessation class. Talk with your doctor, nurse practitioner or pharmacist about the different options and which may be better for you.
- Planning is the key to success. Make a plan for how you will quit (cutting down, cold turkey or using a smoking cessation aid), when you will start (your quit date), and who will help you and be your quit smoking buddy or coach.
- Write out your reasons for quitting and post them someplace where you will see them regularly. Everyone has their own reasons to quit. It may be something like:
- I want to feel better.
- I don’t want to die and leave my family.
- I don’t like how I look when I smoke cigarettes.
- I don’t want to pollute the air my family breathes.
- I’m tired of being out of breath.
- I don’t like how cigarettes make me smell.
- Most people who smoke find that certain places or activities trigger them to smoke. Think about your smoking triggers and what you can do to avoid these places or activities. Then try to think of what you can do to avoid these places or activities. For example, if you always have a cigarette with your morning coffee, switching to tea or drinking your coffee later in the day can help you change your routine.
- Finding it hard to make the change? It may help to see how much money it costs to smoke with the Healthy Canadians Cost Calculator.
- Many people use cigarettes to relieve their stress. But the costs and risks of cigarettes can actually increase the stress in your life. Research suggests that instead of a cigarette, it can be helpful to practice deep breathing. Deep breathing is quick, free and easy to learn:
- For 3 seconds, slowly take a deep breath in through your nose. As you inhale, let your abdomen expand.
- Hold the breath for 3 seconds.
- For 6 seconds, slowly exhale through your mouth. Feel your abdomen moving in.
- Repeat 3 to 5 times.
Deep breathing can not only help you relax, but it can also help reduce cigarette cravings and give you energy because it increases oxygen and blood flow to the brain. Try it the next time you feel like having a cigarette.
For some more ideas, tips and resources, see the following:
- Speak to a Quit Coach at Health811 for quit smoking support by calling 811, TTY 1-866-797-0007.
- Visit Smokers’ Helpline to join an online chat forum with people planning to quit, people who have quit, Quit Coaches and to see more resources. You can also text iQuit to the number 123456 (in Ontario) for quit support.
- Visit the Ontario Ministry of Health’s Quit Smoking website.
- Visit Health Canada’s On the Road to Quitting program.
- Visit QuitMap.ca to find a quit smoking counsellor or group in your community.
- Visit Make Your Home and Car Smoke-Free.
- Visit the Indigenous Tobacco Program website to find resources for First Nations, Inuit, Métis and urban Indigenous peoples.
Tips if you do not feel ready to try
- Write down how you would feel if you could quit. For example, would you feel better about yourself and more in control of your life? Would you be a better role model for your children or loved ones? Would it give you a better chance of being healthy in retirement? Think about what your life would be like if you could quit.
- Keep track of your smoking. Sometimes just seeing how much you are smoking – and being more aware of when you are reaching for a cigarette – can help you cut back. Keep a count of every cigarette you smoke on your cell phone, a piece of paper or your computer.
- Make an appointment with your doctor or nurse practitioner, or speak with your pharmacist about smoking cessation aids and programs that might make it easier for you to quit. Learn about all your options so you can think about what you might do in the future.
- Remember that everyone can change. Just because you are a person who smokes today does not mean you have to be one tomorrow. Millions of people in Canada – including people who smoked for many years – have quit. Every time you try to quit, you are moving closer to the goal of being permanently smoke-free.
- Knowing how much smoking is costing you may help motivate you to quit. Find out at the Healthy Canadians Cost Calculator.
- When you feel ready to start making changes, check out some of these great resources:
- Speak to a Quit Coach at Health811 for quit smoking support by calling 811, TTY 1-866-797-0007.
- Visit Smokers’ Helpline to join an online chat forum with people planning to quit, people who have quit, Quit Coaches and to see more resources. You can also text iQuit to the number 123456 (in Ontario) for quit support.
- Visit the Ontario Ministry of Health’s Quit Smoking website.
- Visit Health Canada’s On the Road to Quitting program.
- Visit QuitMap.ca to find a quit smoking counsellor or group in your community.
- Visit Make Your Home and Car Smoke-Free.
- Visit the Indigenous Tobacco Program website to see resources for First Nations, Inuit, Métis and urban Indigenous peoples.
Tips for avoiding second-hand smoke
- Think of when and where you are exposed to second-hand smoke. Is it at home, in the car or in public places? Once you have identified where and when this is happening, try to think of ways you can change the situation. Could you ban smoking from your home or car?
- Asking friends and family not to smoke around you can be hard. But remember that you are doing this to protect your health. Explain how their smoking can affect your health.
- Focus on your long-term goals, including a long and healthy life with the people you love.
- More resources to help you include:
- How to be a positive influence and help someone quit smoking.
- How to Make Your Home and Car Smoke-Free.
- Visit the Indigenous Tobacco Program website to see resources for First Nations, Inuit, Métis and urban Indigenous peoples.


